Could it Be Fungal Acne?

There’s a rumor going around that those little bumps on your face could be fungal acne. You may even be convinced you have it yourself, desperately watching YouTube video after video of fungal acne routines. Stop. Right. Now.
According to board-certified dermatologists, fungal acne isn’t even acne. It’s a phantom diagnosis. Fungal acne has nothing to do with either fungus or acne. It’s basically an infection of the hair follicles on the face or body that leads to papules and raised bumps resembling pimples.
Let us break it all down for you.
WHAT IS FUNGAL ACNE?
Fungal acne is an infection of the hair follicle. It is a condition technically referred to as pityrosporum folliculitis or Malassezia folliculitis. People often mistake it for regular acne because of its similar appearance. But unlike acne, it’s caused by excess yeast known as Malassezia.
Malassezia lives on our skin. It’s totally normal – and healthy! But when those yeast levels increase, especially during hot weather or when you’re sweaty, that’s when fungal acne occurs.
“High yeast levels promote inflammation, which, in turn, manifest on the skin as pus bumps,” explains Joshua Zeichner, the director of cosmetic and clinical research at Mount Sinai Hospital in New York City.
HOW TO TELL IF IT’S REGULAR ACNE OR FUNGAL ACNE?
Besides their technical differences, they do have other more visible differences. For example, fungal acne can be contagious because yeast is involved, whereas regular acne isn’t. That’s why it’s not a good idea to share towels or beauty tools if you have this condition.
Look for small whiteheads or blackheads that are around one millimeter in circumference. That’s a sign it could be fungal acne.
Other differences include itching and inflammation. And it usually takes place on the body rather than the face.
“Inflammatory acne tends to affect the face and is usually either due to increased oil production, follicular plugging, excess bacterial growth of propionibacterium acnes, or hormonal changes,” says cosmetic dermatologist Shereene Idriss. “Fungal acne, on the other hand, frequently appears as uniform papules and pustules on the chest and back or in areas of occlusive clothing.”
So if you’re experiencing breakouts on your chest, back, or upper arms, there’s a high chance it could be fungal acne.
WHAT CAUSES FUNGAL ACNE
Here are a few reasons why you might be getting fungal acne.
- Sweat
Sitting around in sweaty clothes is a recipe for fungal acne.
- Heat and humidity
Fungal acne thrives in moist environments with sweat and heat.
- Overuse of antibiotics
“In certain circumstances—such as long-term use of topical and/or oral acne antibiotics—the normal skin flora is wiped out by the antibiotics, and so the yeast flourishes, causing inflammation and fungal acne,” explains dermatologist Morgan Rabach.
- Bodily contact
Because fungal acne can be contagious, it’s possible to pass it on via shared use of towels or any form of bodily contact with someone who has fungal acne.
HOW TO TREAT FUNGAL ACNE STEP-BY-STEP
Once you know for sure it’s fungal acne, treating it isn’t that hard.
- Use an Anti-Dandruff Shampoo
Anti-dandruff shampoos are the simplest tool for getting rid of fungal acne. They contain an active ingredient called zinc pyrithione, which is antifungal and excellent for fighting fungal acne. You can use it as both a facial and body cleanser.
“Apply, let it sit, and lather it up while you sing the alphabet before rinsing it off,” Zeichner advises. “The shampoo needs enough contact time on the skin for it to exert its effect.”
Try making it a part of your daily routine to keep skin clear and blemish-free.
- Exfoliate Dirt and Oil
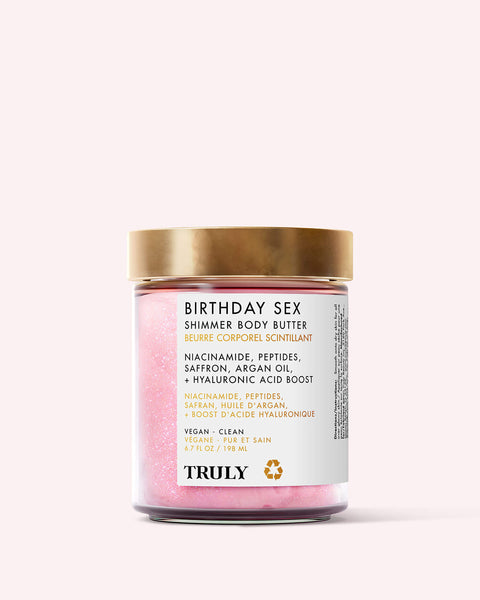
The same things as regular acne may not cause fungal acne, but it’s still important to keep your skin clean and exfoliated. See, dead skin cells, dirt, and oil can all contribute to yeast growth. With regular exfoliation, you can slough away the grime and lessen the chance of getting fungal acne. Try Truly’s Blueberry Kush Hemp Body Scrub to detoxify and illuminate your skin.
- Use a Tea Tree-Formulated Treatment
Tea tree oil is packed with antiseptic and antifungal properties, making it a perfect fungal acne treatment. Dilute 1-2 drops of tea tree oil with several drops of a carrier oil like almond oil, then apply topically to affected areas.
Alternatively, try a tea tree-formulated skincare product like Truly’s Black Jelly Blemish Treatment Body Serum. Made with tea tree, witch hazel, and black charcoal, it’ll zap fungal acne in no time.
- Try an Anti-Fungal Cream
If you’re suffering from fungal acne, you could try looking for an over-the-counter cream with active ingredients that reduce yeast overgrowth.
“Look for an antifungal cream with econazole nitrate, ketoconazole, or clotrimazole, and apply it to the affected area twice daily,” says dermatologist Dr Hadley King. “Don’t use topical or systemic antibiotics. This can deplete bacteria on the skin and allow yeast to grow unchecked.”
FUNGAL ACNE PREVENTION TIPS
While you can’t make yourself utterly immune to fungal acne, there are a few things you can do to reduce your chances of getting it.
Most importantly, take a shower or at least swipe over your skin with a salicylic-formulated wipe after sweaty workouts. Sweating leads to excess yeast production. So keeping your skin sweat-free can help significantly in preventing fungal acne.
Another important one: steer clear of heavy moisturizers and oils. These only make fungal acne worse, as they create a moist environment on the skin that allows yeast to grow.
You’ll also slash your chances of contracting these itchy bumps by wearing loose-fitting, breathable clothing. Tight clothing traps sweat and causes friction on the skin, which often leads to yeast overproduction.
And don’t forget, avoid sharing towels or any bodily tools with people who have fungal acne. They could pass it on to you!
WHEN TO SEE A DERMATOLOGIST
If your symptoms persist after 2-3 weeks and you’ve tried all the steps above, it’s time to book an appointment with a dermatologist. They’ll be able to confirm your diagnosis and provide a treatment plan for you, possibly with an oral antifungal medication prescription.